Overview
Medical personnel are challenged with preventing skin injury in the perioperative environment due to prolonged periods of patient immobility, compromised circulatory function under anesthesia, and preexisting conditions of many surgical patient populations. While great strides have been made in protecting the patient from skin injury, it is an issue that still needs to be addressed. These skin injuries may result in extended hospital stay, increased medical costs and prolonged morbidity. The healthcare facility may also incur financial and legal ramifications from these injuries.1,2
Impact of Pressure Ulcers on the Surgical Patient
Length of Hospital Stay
The length of hospital stay varies depending upon the type of surgical procedure being performed. However, this may increase by 3.5 to 5 days on average when a pressure ulcer is present.3,4 In some unusual cases, the adjusted length of stay for pressure ulcers may be as high as 15.6 days.5,6
Cost Factors
Cost factors for pressure ulcer treatment have a tremendous impact on the patient and healthcare facility. The average range per incident costs $5,000-$60,000,3,5-13 depending upon the severity of the pressure ulcer and the type of treatment required. Actual cost can reach as high as $90,000 for one incident.10
Nursing care costs and time can increase by 50% for each pressure ulcer acquired during a surgical procedure.10,12 Furthermore, cardiac and vascular surgery patients account for approximately 45% of the total hospital pressure ulcer treatment costs.10
A prevalence study conducted at a large U.S. hospital provides actual numbers and not merely statistical estimates. The average length of stay for those patients acquiring pressure ulcers increased by 6.5 days and cost an additional $12,000 for treatment.10 Unfortunately, the average reimbursement rate per patient from insurance and Medicare/Medicaid was less than $1,600. Therefore the hospital was losing more than $10,000 per pressure ulcer incident.10
In the United States, perioperatively acquired pressure ulcers cost $750 million-$1.5 billion per year on average.10,14
Additional Complications
Patients who have pressure ulcers may be predisposed to other complications. Those complications may include, but are not limited to: bacteremia,7 squamous cell carcinoma,7 sinus tract formation,7 osteomyelitis,7,11,15 pyarthroses,11 amyloidosis,11 and sepsis.11,15
Patients with pressure ulcers are impacted emotionally and financially, as well as physically.10,11 They are subject to pain, disfigurement, additional treatment, increased hospital stay, loss of income, loss of independence and possibly even loss of life.4,9,11
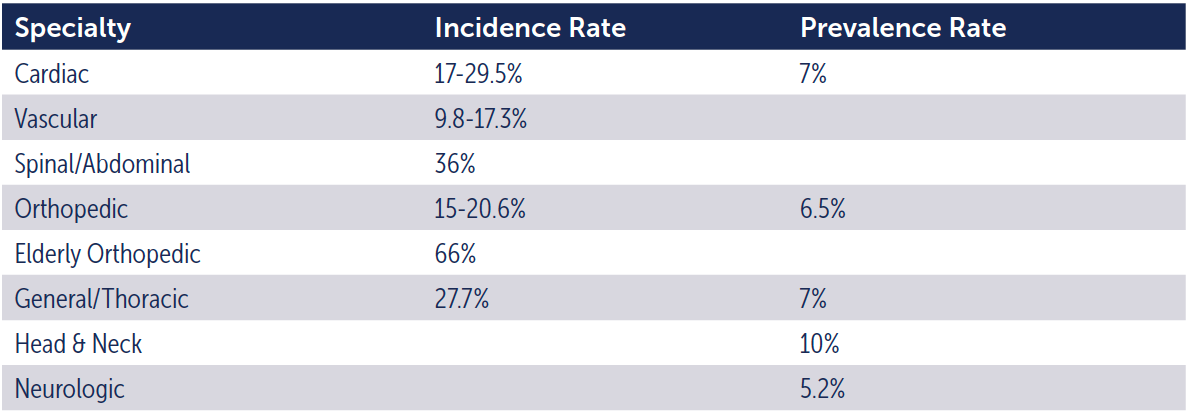
Surgical patients are more susceptible to developing pressure ulcers than general acute care patients. This is due to many risk factors only present in the intraoperative environment. The incidence rate (the number of new cases of disease occurring in a population during a defined time interval) for surgical patients ranges from 12-66%.3,9-11,15-21 On average, the prevalence rate (a percentage of a population that is affected with a particular disease at a specified time) for surgical patients is between 3.5-29%.10,22,23
Furthermore, there are many opportunities for patients to develop pressure ulcers depending upon the type of procedure being performed. These specialties have differing incidence and prevalence rates. See Table 1.
Table 1. Incidence and Prevalence by Specialty3,8-10,12,15,18,19
Length of Surgery
As the length and time of surgery increase, the incidence and percentage of patients with pressure ulcers also increases.9 See Table 2.
Table 2. Prevalence Rate Based on Length of Surgery3,4,18,28
Due to their negative impact, it is imperative to employ best practices that will assist in preventing pressure ulcers in surgical patients. In order to do this effectively, healthcare professionals need to recognize the risk factors and mechanisms contributing to pressure ulcer formation and identify them accurately if they do occur.
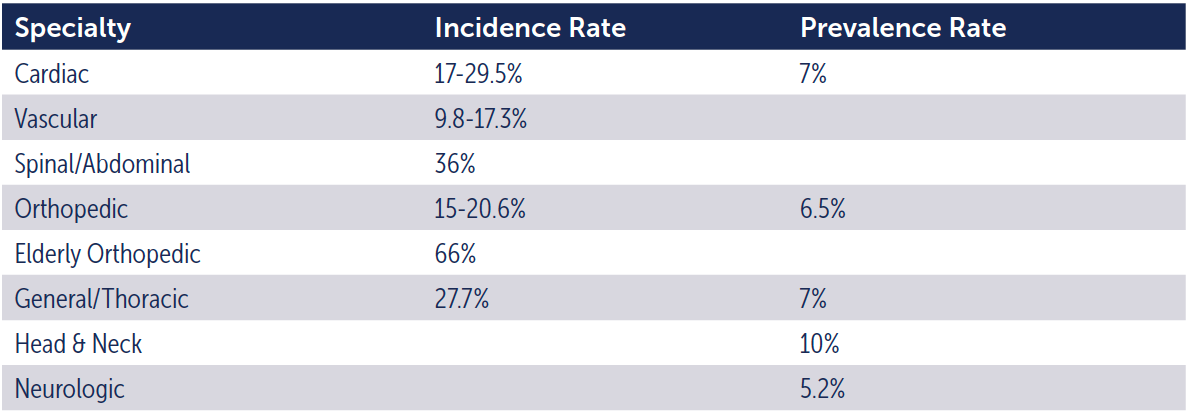
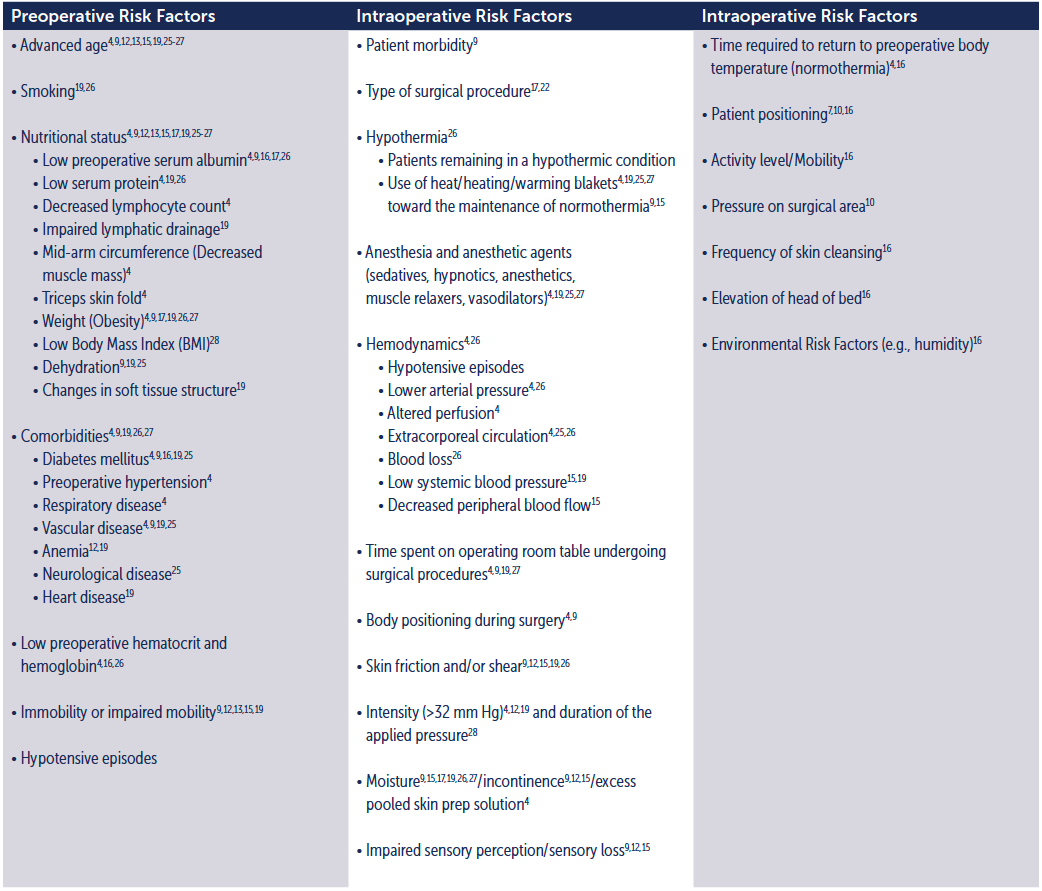
Risk Factors for the Development of Pressure Ulcers
Approximately 95% of all pressure ulcers are preventable IF early risk assessment is performed and appropriate interventions are implemented.13
There are a substantial number of risk factors for developing pressure ulcers perioperatively. Many studies have attempted to identify the most accurate risk indicators for pressure ulcer development in the surgical patient. See Table 3.
Table 3. Risk Factors for Pressure Ulcers in the Surgical Patient
Mechanisms Contributing to the Formation of Pressure Ulcers
Pressure ulcers have multiple causes. Their development and severity may be affected by vascular occlusion, ischemia and/or pressure intensity. Pressure ulcers develop when sustained mechanical occlusion of the vascular network occurs. Extended periods of uninterrupted pressure and shear occlude blood and lymphatic circulation, causing deficient tissue nutrition and a buildup of waste products due to ischemia. Blood vessels collapse and thrombose if the pressure is not relieved over time.
Once occlusion of the blood flow has occurred, ulceration continues the process. When tissues have been compressed for prolonged time periods, tissue damage continues to occur even after the pressure is relieved. Studies suggest an inverse relationship between pressure intensity and duration (time) of pressure in pressure ulcer development.7 Therefore, tissue damage can be produced by low pressures over an extended period of time or high pressures for shorter periods of time.4,10,12,15,23,25,29
It is important to note that the patient’s tolerance to pressure during surgical procedures can be affected by factors that may cause changes in metabolism and circulation such as anesthesia, surgical trauma, patient age, and other preexisting conditions.30 As a result, the patient’s own body weight upon bony prominences is directly capable of creating injury situations. Figure 1 provides a visual illustration of the pressure ulcer development cycle.
Pressure ulcers which originate during the perioperative environment may appear within as little as a few hours postoperatively. However, the majority typically present one to three days postoperatively.4,10,26 These surgically-associated late onset pressure ulcers are often mischaracterized as energy-related “burns”.31 Gendron stated that “it is precisely the lack of recognition of their [pressure ulcers’] true nature that has guaranteed their continuance.”32
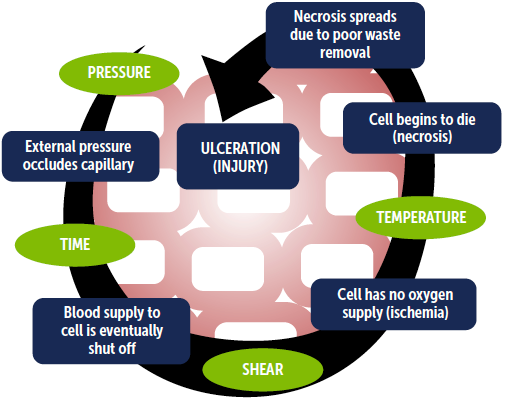
Additional situational factors that augment the risk of pressure ulcer development in the perioperative setting have been identified. They include shear, pressure, temperature and time as discussed below.
- The presence of shear may decrease the time that tissue can remain under pressure before ischemia occurs.
- The sustained high pressure from specific patient positions and/or various devices such as use of supports and straps, pneumatic tourniquets, and unyielding electrode adhesives for an extended time (>2-3 hrs) may shorten the time to pressure ulcer development.1,2
- Elevated tissue temperatures increase the oxygen consumption rate of the local cells, thereby shortening the time to death from ischemia.
- The severity of the ulcer is determined by the length of time pressure is applied to any given location. The probability of developing a pressure ulcer increases with the duration and intensity of the pressure and shearing force acting upon the tissue during surgery.33 See Figure 2.
Figure 1. The Pressure Ulcer Development Cycle
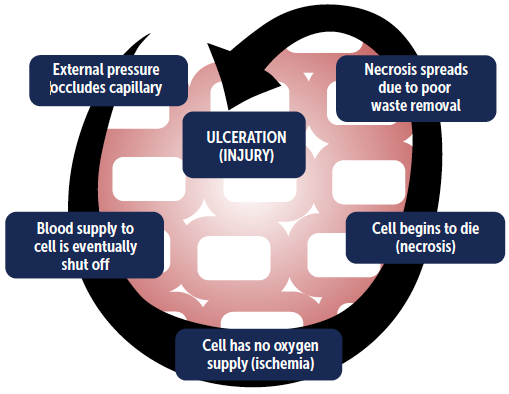
Figure 2. The Accelerated Cycle of Pressure Ulcer Development
Is there anything else I need to know?
If you have any questions about the AAMI Ratings of surgical gowns or drapes provided for your use in the OR, ask your supervisor. Another great resource is the Association of periOperative Registered Nurses (AORN). The AORN Guidelines for Perioperative Practice offer comprehensive guidance to the types of gown protection needed for operative and other invasive procedures.
For a handy reference, download our Simplified Guide to Gown Guidelines poster.