Unfortunately even with the best of intentions, healthcare workers do not always wash and disinfect their hands as often as they should.
This less than perfect hand hygiene performance can pose a serious risk to patients because as stated by Dr. Julie Gerberding, director of the Centers for Disease Control (CDC), “Clean hands are the single most important factor in preventing the spread of dangerous germs and antibiotic resistance in healthcare settings.1
While the use of gloves does not eliminate the need for hand hygiene, likewise, the use of hand hygiene does not eliminate the need for gloves. Gloves reduce hand contamination by 70 percent to 80 percent, prevent cross–contamination and protect patients and healthcare personnel from infection.
The importance of gloves, masks, and other personal protective apparel cannot be overestimated in preventing infection in healthcare settings. They, along with hand hygiene, are the first line of defense in preventing the spread of infection from person to person within healthcare settings.
Research & Reports
Nosocomial Infections and Multidrug-resistant Organisms in Germany (Deutsches Aerzteblatt International)
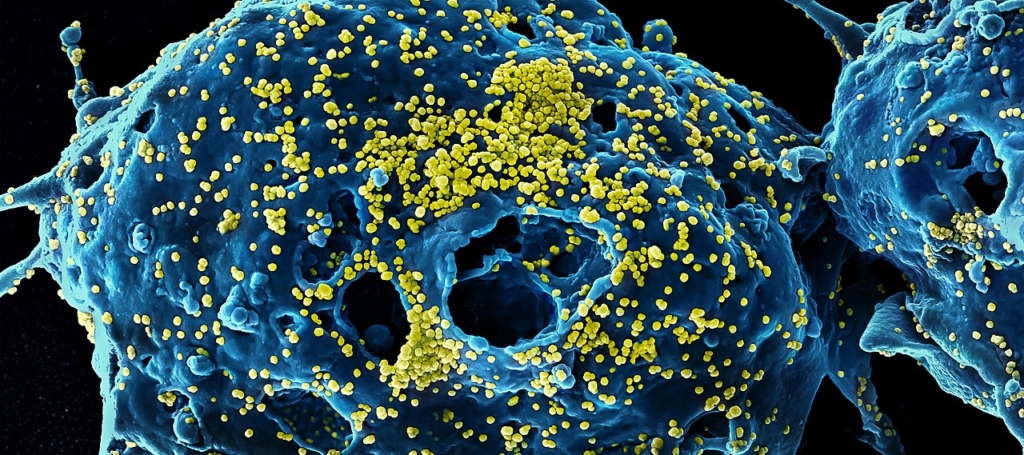
Research published in Deutsches Arzteblatt International said infections are among the most frequent complications of a stay in a hospital in Germany, and they raise complication and mortality rates. Based on data from the Hospital Infection Surveillance System, the study showed an incidence of almost 60,000 newly acquired infections annually in Germany’s intensive care units. Christine Geffers of the Institut fur Hygiene und Umweltmedizin and co-author Petra Gastmeier also found that while the percentage of patients in intensive care who have methicillin-resistant Staphylococcus aureus species has been stable for years, the number with extended-spectrum beta-lactamase-producing E. coli and Klebsiella pneumoniae is increasing.
Electronic Prediction Rules Methycillin Resistant Staphylococcus Aureus Colonization (Journal of Infection Control and Hospital Epidemiology)
Researchers from the University of Chicago and colleagues concluded that many steps hospitals take to minimize the number of methicillin-resistant Staphylococcus aureus infections, including engaging in surveillance for MRSA colonization, are costly and can result in false-positive test results. According to the scientists, whose work was published in Infection Control and Hospital Epidemiology, the performance of this technique would be enhanced if patients who are at high risk for colonization could be easily targeted. The investigators studied 23,314 patients and came up with five MRSA prediction rules that could be used to identify the 30 percent of patients who account for approximately 70 percent of all MRSA-associated patient-days.
Read More
Small Molecule Inhibitors of Staphylococcus aureus RnpA Alter Cellular mRNA Turnover, Exhibit Antimicrobial Activity, and Attenuate Pathogenesis (PLOS Pathogens)
Researchers have shown that stopping MRSA’s ability to degrade RNA can inhibit its spread, both in the laboratory and in infected mice, according to a report published in PLoS Pathogens. Scientists led by Paul Dunman of the University of Rochester Medical Center especially focused on RnpA, a molecule they found to be involved in the RNA degradation process. Specifically, the team isolated RNPA1000, and in tests on mice, 50 percent of those treated with a large dose of the molecule survived while all of the mice in the control group died. The scientists said inhibiting degradation might cause the bacteria to be overcome by an onslaught of confusing instructions that should have been turned off.
Social and cultural dimensions of hygiene in Cambodian health care facilities (BioMed Central Public Health)
Pascale Hancart-Petitet of the Institut Pasteur du Cambodge in Phnom Penh, Cambodia, and colleagues reported in BMC Public Health on the social and cultural factors shaping hygiene practices in Cambodian health care settings. According to the researchers, the frequency of bloodborne pathogen-related infections is thought to be high in developing Southeast Asian countries, but the social-cultural logics contributing to the risks of transmission are rarely studied. The researchers conducted qualitative surveys of 319 participants and found that hygiene practices were burdened in part by a lack of adequate materials and equipment.
Infection Acquisition Following Intensive Care Unit Room Privatization (Archives of Internal Medicine)
Placing intensive care unit patients in private rooms may help lower the risk of infection. In the study, Teltsch and colleagues analyzed data from 19,343 ICU admissions between 2000 and 2005 at two Montreal hospital centers, one of which switched to only private ICU rooms in March 2002. They found that the combined risk of a patient acquiring an infection such as MRSA, vancomycin-resistant Enterococcus species and Clostridium difficile dropped by 54 percent after the transition to private rooms. Additionally, the researchers found that the average patient in a private room stayed in the ICU 10 percent fewer days after the conversion.